Cancer is a wide spectrum of diseases characterized by uncontrolled cell growth. Studying the mechanisms by which cancer cells replicate and metastasize will drive scientific advancements and breakthroughs in cancer research. Most cancers are characterized by cells that grow uncontrollably and form a tumor. They typically divide more frequently than normal cells and lose the ability to undergo programmed cell death, also known as apoptosis.

Cancer Biology
Types of Cancer
Solid tumor cancers are the most common, particularly in tissues and organs like the breast, lung, prostate, skin, and bladder. Cancers that are not considered solid cancers are often grouped under blood cancers. The three main types of blood cancers are myeloma, lymphoma, and leukemia and are named after the system they affect or where they originated, such as the bone marrow, lymphatic system, and blood, respectively. Cancers that affect the same system tend to share common traits and symptoms.
Myeloma, often referred to by its most common form ‘multiple myeloma,’ originates in the bone marrow and affects plasma cells. These can accumulate in the marrow and cause damage to the bone. Lymphomas affect the lymphatic system, and lymphocytes can grow and accumulate in lymph nodes, the spleen, or other tissues. In leukemia, the bone marrow produces mutated cells, and these cells are spread into the bloodstream.
Understanding the mechanisms by which these cancer cells spread and avoid detection are crucial for novel immunotherapies.
Mechanisms of Cancer Growth
Cancer cells undergo cell division more frequently than the cells in normal tissue, and they often have lost the ability to undergo programmed cell death. Additionally, they can metastasize to other regions of the body. Major causes of disordered cellular programming in cancer can result from internal genetic and epigenetic changes1.
Point mutations, deletions, duplications, insertions, translocations, chromosome aberrations, viral infections, and epigenetic inactivation represent various types of potentially cancer-causing events. These mechanisms may affect the DNA sequence, promote aberrant cell growth, change the function and regulation of the gene products, or lead to a loss of function. The products of tumor suppressor genes commonly control cell division and genetic stability.
Additionally, accumulation of DNA damage has been linked to cancer, and genetic deficiencies in specific DNA repair genes are associated with tumor-prone phenotypes. In addition to mutations, which can be either inherited or somatically acquired, epigenetic silencing of DNA repair genes may promote tumorigenesis.
A number of external factors can cause uncontrolled cell division and tumor growth including UV radiation, hormones, pollutants, environmental toxins, and smoking2. Most of these have been linked to DNA damage, defects in DNA repair mechanisms, or both.

Cancer Metabolism
Normal cells typically generate only about 30% of energy from glycolysis, while in contrast most cancers rely on glycolysis for energy production (called the Warburg Effect). In addition, a minority of cancer types rely on oxidative phosphorylation as the primary energy source. Even in these cases, the use of glycolysis as an energy source rarely exceeds 60%. A few cancers use glutamine as the major energy source, partly because it provides nitrogen required for nucleotide (DNA, RNA) synthesis. These metabolic states produce various metabolites and conditions that are beneficial to the tumor and are active areas of research3.
Angiogenesis
Angiogenesis is the formation of new blood vessels that supply oxygen and nutrients to cells and tissues. Angiogenesis inhibitors are commonly used as cancer treatments because tumors that lack circulatory support have difficulty growing and spreading.
Our LEGENDplex™ Human Angiogenesis Panel can be used to detect various factors and cytokines involved in cell adhesion and angiogenesis.
Metastasis
Metastasis is the spread of cancer to other locations in the body. The dispersed tumors are called metastatic tumors. Metastasis is common in the late stages of cancer, and it can occur via the blood, the lymphatic system, or both. The typical steps in metastasis are local invasion, intravasation into the blood or lymph, circulation through the body, extravasation into the new tissue, proliferation, and angiogenesis.
Tumor Microenvironment
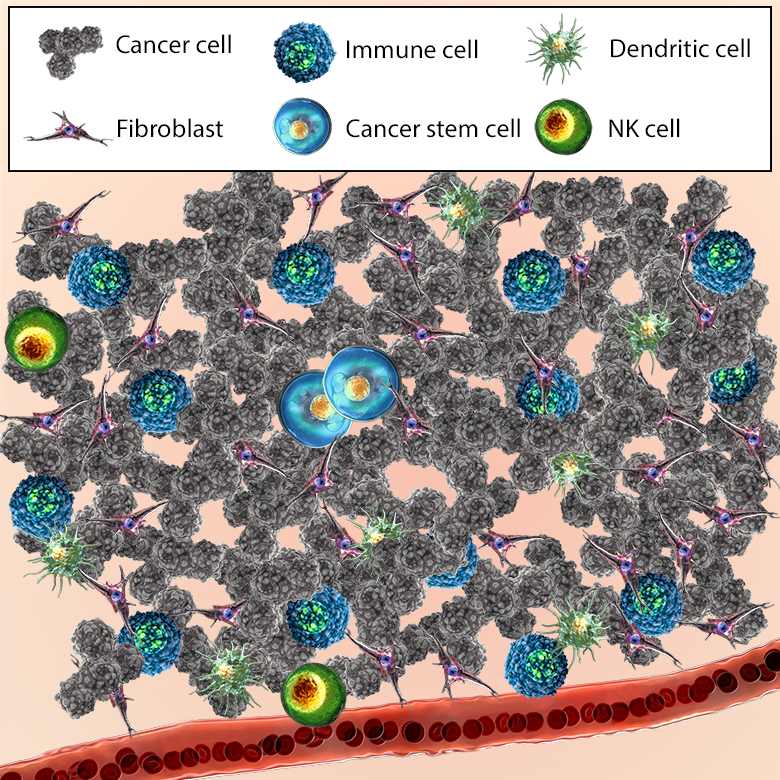
The Tumor Microenvironment (TME) is a term used to represent the collection of cells, factors, and physiological conditions of the tumor and surrounding tissues. Several reports describe molecular interactions between cancer cells and their microenvironment. In addition, the TME has been shown to have an important role in malignancy5.
The immune system surveils and eliminates tumor cells through the production of inflammatory cytokines, recognition of tumor antigens by dendritic cells, or activation of natural killer cells. Production of cytokines such as TNF-α, IFN-γ, and IL-1β by macrophages and T cells enhances inflammation through additional recruitment of immune cells.
If tumor cells escape immune detection, they can grow and spread to other tissues. This can be done through a variety of mechanisms including the shedding of tumor recognition antigens, tumor associated macrophage (TAM) or myeloid derived suppressor cell (MDSC)-induced immunosuppression, or development of a microenvironment that supports T cell apoptosis6.
Tumor cells can leverage different cellular and non-cellular components of the microenvironment to promote growth and survival under hostile conditions (such as low oxygen and diffusion, and high acid concentration)4,7. These conditions are modulated and maintained by soluble factors such as chemokines, cytokines, growth factors, or exosomes. Endothelial cells (ECs) build up the inner layer of blood vessels in a growing tumor. Tumor endothelial cells (TEC) can benefit tumor cells by promoting angiogenesis, progression, and metastasis. Fibroblasts can also be commandeered by the tumor, changed into carcinoma associated fibroblasts (CAFs), and utilized as a source for growth factors that support angiogenesis6.
Considerable research is ongoing as to the effect of these interactions on the surveillance and treatment of cancer cells8. Understanding how the TME affects cancer progression is expected to make new targets available for cancer cell characterization and cancer treatment5.
Learn more about immune cells and other important cell types in the tumor microenvironment.
References
- Lahtz C. & Pfeifer G.P. (2011). Epigenetic changes of DNA repair genes in cancer. Journal of Molecular Cell Biology. 3 (1): 51–8. doi:10.1093/jmcb/mjq053. PubMed.
- Kocarnik, J.M. et al. (2022). Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life Years for 29 Cancer Groups From 2010 to 2019. A Systematic Analysis for the Global Burden of Disease Study 2019. JAMA Oncology. 8 (3): 420–444. doi:10.1001/jamaoncol.2021.6987. PubMed.
- Audrito, V. et al. (2019). NAD-Biosynthetic and Consuming Enzymes as Central Players of Metabolic Regulation of Innate and Adaptive Immune Responses in Cancer. Frontiers in Immunology. 10. 10.3389/fimmu.2019.01720. PubMed.
- Jahanban-Esfahlan R. et al. (2017). Modulating tumor hypoxia by nanomedicine for effective cancer therapy. J Cell Physiol. 2017;233:2019–31. PubMed.
- Sounni N.E. & Noel A. (2013). Targeting the tumor microenvironment for cancer therapy. Clin Chem. 2013;59:85–93. PubMed.
- Oliver A.J. et al. (2018). Tissue-dependent tumor microenvironments and their impact on immunotherapy responses. Frontiers in Immunology. 2018;9:70. PubMed.
- Baghban, R. et al. (2020). Tumor microenvironment complexity and therapeutic implications at a glance. Cell Communication and Signaling: CCS vol. 18,1 59. doi:10.1186/s12964-020-0530-4. PubMed.
 Login/Register
Login/Register 






Follow Us